NGS Panels Demonstrate Value in Brain Tumor Studies
Introduction
Founded in 1885, Yonsei University College of Medicine Severance Hospital has grown to become one of the largest university hospitals in South Korea. It is at the forefront of medical practice and focused on becoming the medical hub of Northeast Asia. Hospital clinicians are now performing more than 1200 clinical trials per year. Its pathology team also leads the way in using next-generation sequencing (NGS) for clinical studies to identify and stratify disease.
Se Hoon Kim, MD, PhD is a Professor in the Department of Pathology at Severance Hospital. He specializes in neuropathology and evaluating new tools for reliable, rapid, and informative diagnosis of brain tumors, such as gliomas. Gliomas comprise approximately 30% of all brain and spinal cord tumors and 80% of all malignant brain tumors.1 Mutations in isocitrate dehydrogenase (IDH)1 and 2 are among the most frequent mutations in low-grade and secondary high-grade gliomas.2 IDH mutation detection and identification are important in clinical care and prognosis of glioma patients. Patients with IDH1 and IDH2 mutant tumors have prolonged survival compared to those with wild-type IDH gliomas.3 Although IDH1 gliomas are less aggressive, they are therapy resistant.
Together with Department Fellow, Kiyong Na, MD, Dr. Kim conducted a comparison study with existing gold standard methods and the TruSight Tumor 170 assay on the NextSeq™ 550 System to detect IDH mutations and other cancer-related variants in glioma biopsies.Current tools to detect IDH mutations include immunohistochemistry (IHC) and pyrosequencing. TruSight Tumor 170 is a targeted panel that supports analysis of DNA and RNA, covering a wide range of genes and variants associated with solid tumors. The NGS data compared favorably with these current approaches. iCommunity spoke with Dr. Kim and Dr. Na about their study and the role NGS might play in tumor characterization and diagnostics in the future.
Se Hoon Kim, MD, PhD is a Professor in the Department of Pathology and Kiyong Na, MD is a Department Fellow at Severance Hospital in Seoul, South Korea.
Q: What is the focus of your technology evaluation studies for assessing brain tumors?
Se Hoon Kim (SHK):We’re evaluating new technologies to determine their speed and reliability and whether the information they provide could be clinically useful in identifying known genetic markers in neuropathology specimens. Our pathology lab currently uses qPCR, Sanger sequencing, and fluorescent in situ hybridization (FISH) to assess tumor biopsy samples. Companies and research laboratories throughout the world are continually developing new analysis technologies. We perform correlation studies to determine the accuracy, reliability, cost effectiveness, and potential turnaround time of these new approaches in comparison to our gold standard procedures.
Q: When did you begin using TruSight Tumor 170 and the NextSeq 550 System in your brain studies?
Kiyong Na (KN): We began using the NextSeq 550 System in 2017 when the South Korean government offered selective reimbursement of NGS-based tests.
SHK: Rather than perform studies to identify novel mutations, we use NGS-based tests to identify or confirm markers that show promise for diagnostics or personalized treatments.
KN: For example, we reassessed the subtype of a tumor sample with TruSight Tumor 170 BRAF mutation data. In another case, we were also able to reassess a loss of heterozygosity (LOH) assessment with TruSight Tumor 170 data.
We also use the NextSeq 550 System to detect fusion variants, epidermal growth factor receptor (EGFR) amplification, and EGFRvIII mutation, which are overexpressed in glioblastomas. Previously, we used FISH to detect EGFR amplification. Using TruSight Tumor 170 and the NextSeq 550 System, our detection of EGFR amplification aligns with globally reported trends.
Q: What were the parameters of your glioma biopsy sample studies with the TruSight Tumor 170 Panel and the NextSeq 550 System?
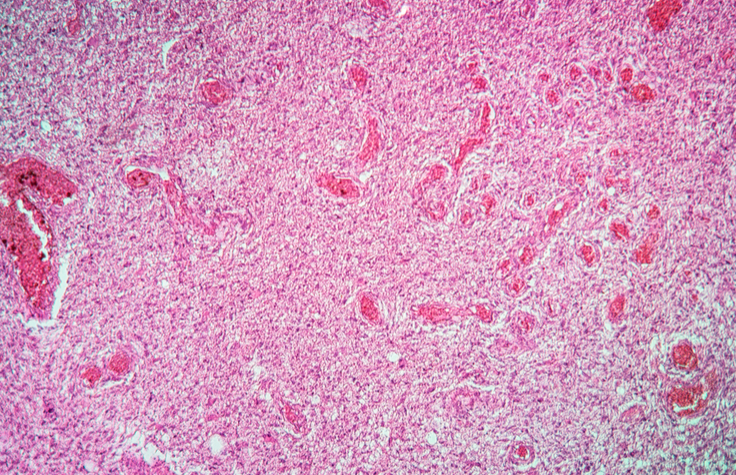
SHK: We performed a comparison study between TruSight Tumor 170 on the NextSeq 550 System and other molecular diagnostic methods we’ve been using to assess clinically relevant genetic variants in a specific subset of brain tumors known as diffuse gliomas. Diffuse gliomas are the most common brain tumors in adults and are characterized by diffuse infiltration of tumor cells in the neuropil; the dense network of interwoven neuronal and glial cell processes.
KN: We collected every diffuse glioma sample that we received during the last year. We reanalyzed more than 200 samples with TruSight Tumor 170 on the NextSeq 550 System and compared its variant detection performance with our standard methods.
Table 1: Comparison study data-IHC, pyrosequencing, and NGS analysis of diffuse glioma samples.
Gene/Variant/Assay |
Comparator Assay |
Next-Generation Sequencing |
|||||
|---|---|---|---|---|---|---|---|
IDH1 IHC |
135 |
R132H |
Other Mutant |
Wild Type |
Concordance Rate |
||
R132H mutant |
38 |
38 |
0 |
0 |
100% |
||
| R132H wild type | 97 |
0 |
0 |
97 |
100% |
||
BRAF IHC |
17 |
V600E |
Other mutant |
Wild Type |
Concordance Rate |
||
VE1 mutant |
5 |
5 |
0 |
0 |
100% |
||
VE1 wild type |
12 |
0 |
1 |
11 |
100% |
||
IDH Pyrosequencing |
48 |
IDH1 mutant |
IDH2 mutant |
Wild Type |
Concordance Rate |
||
| IDH1 mutant | 0 |
0 |
0 |
0 |
100% |
||
| IDH1 wild type | 48 |
|
0 |
0 |
48 |
100% |
|
| IDH2 mutant | 0 |
0 |
0 |
0 |
100% |
||
| IDH2 wild-type | 48 |
0 |
0 |
48 |
100% |
||
TERT Pyrosequencing |
135 |
TERT mutant |
Other mutant |
No Result |
Concordance Rate |
||
C228T mutant |
53 |
53 |
0 |
0 |
100% |
||
C250T mutant |
17 |
17 |
0 |
0 |
100% |
||
Wild type |
65 |
0 |
3 |
62 |
100% |
||
Q: What were the results of this comparison study with diffuse glioma samples?
KN: The most important target gene in our research was IDH. Previously, we used IHC or pyrosequencing to analyze the diffuse glioma samples in the collection. TruSight Tumor 170 successfully reported the presence or absence of IDH variants with 100% concordance with previous analysis approaches (Table 1). All detected IDH variants were in R132H, which is known to be the most common IDH mutation in brain tumors. It is encouraging that TruSight Tumor 170 stably detected the most common IDH mutation. In addition, TruSight Tumor 170 identified similar TP53 and BRAF mutation levels as those seen using immunochemistry methods.
We also compared pyrosequencing and NGS data of TERT promoter mutation status. C228T and C250T variants are the most common variants of the TERT promoter region. TruSight Tumor 170 data correlated well with conventional pyrosequencing and also detected several minor variants that were not included in the pyrosequencing data. The detection of the TERT promoter mutation is crucial for diffuse glioma. However, C228T variants of the TERT promoter region were often observed to be excluded in *.vcf files due to suboptimal read depth. As a result, we had to take a very close look at the Integrated Genome Viewer (IGV) on this genomic region for the variant.We were keen to figure out what caused the suboptimal coverage on the region and found that lower read depth of the TERT promoter region was also reported with other NGS panels.It has been suggested that very high GC content of the TERT promoter region would be related to that issue.
One interesting finding concerns 1p/19q codeletion. With TruSight Tumor 170, we observed that most of the oligodendrogliomas harbored significant copy number loss of 1p and 19q genes, including NRAS1, MYCL1 (1p) and CCNE1, AKT2, ERCC1, and ERCC2 (19q). This correlated well with our FISH data in oligodendroglioma samples. The data suggest that this clustered copy number loss may reflect the deletion of 1p and 19q genes. This data would have been more meaningful if TruSight Tumor 170 included more genes located within the 1p and/or 19q regions.
" It is encouraging that TruSight Tumor 170 stably detected the most common IDH mutation...and similar TP53 and BRAF mutation levels as those seen using immunochemistry methods."
Q: How will the broader TruSight Oncology 500 panel solve some of the issues you found with the TruSight Tumor 170 panel?
SHK: The TruSight Tumor 170 is a focused panel. As a result, it has some limitations in performing the comprehensive genetic profiling that is required when assessing brain tumors.
We believe that these issues have already been resolved with the recent introduction of the TruSight Oncology 500 panel, which is a pan-cancer panel that covers more than 500 genes. It is more comprehensive than TruSight Tumor 170 and enables various types of biomarkers to be analyzed simultaneously, including single nucleotide variants (SNVs), indels, amplifications, fusions, and splice variants. It also measures tumor mutation burden (TMB) and microsatellite instablity (MSI) status, which are essential biomarkers for supporting future immuno-oncology therapies.4
Q: How did you analyze TruSight Tumor 170 data in the study?
KN: Our analysis of TruSight Tumor 170 data is based on *.vcf files. We set up a few filtration standards internally with other members of Yonsei pathology. The final selection of variants is done manually using the internal filtration and selection standards.
In some instances, we found that variant calls could be out of standard nomenclature due to the confusion of the variant call algorithm between single nucleotide deletion and duplication. This might be solved by incorporating data from the 1000 Korean genome project into the data filtration process or using the data as normal reference data. This would significantly increase the accuracy of somatic variant calls in Korean samples.
Q: Is there value in combining NGS with methylation arrays to assess brain cancer samples?
SHK: I believe somatic mutation profiling using NGS will become routine in clinical practices. I also believe that comprehensive genetic profiling of brain tumors would benefit from methylation array analysis. This is exemplified by Dr. David Capper’s projects at the German Cancer Research Center (DKFZ) using Infinium™ HumanMethylation450K and MethylationEPIC arrays for methylation analysis of brain tumor samples.5
The issue we have in Korea is that methylation arrays are not yet reimbursed here, limiting the funding we can obtain to perform clinical research studies investigating their use in identifying brain cancer mutations. There are also some regulatory issues of transporting or sharing clinical/genetic data internationally when necessary to support international collaborations.
"We are enthusiastic about the new TruSight Oncology 500 panel, which is more comprehensive and enables various types of biomarkers to be analyzed simultaneously."
Q: How are regulations and reimbursements for NGS genetic assessments in Korea evolving?
SHK: According to the Korean government’s original announcement, there will be a review process occurring in late 2018 for the selective reimbursement program of NGS-based clinical tests. This issue has a high profile in Korea among brain tumor patients and families. Patient advocacy groups are pushing for individual access to high-tech diagnostic tests, such as NGS, as well as to new brain tumor drugs. These are not currently provided under the public health care support system regulated by the Korean government.
Q: What does the democratization of NGS mean to you?
SHK: I think there’s a positive aspect, if you mean that democratization would provide universal and general access to NGS for the benefit of average patients. It would close the gap between bench and bedside by making access to comprehensive NGS data and use of NGS analysis technology easily available.
However, I have some concerns regarding the availability of high-tech medical tools in the world. The current gap in the availability of NGS or other high-tech medical tools has the potential to become wider in the future between different economic classes, and between underdeveloped countries and wealthy countries. The same story could occur with the availability of new, yet expensive, treatments and drugs. I’m concerned about how to limit the widening gap or polarization in the availability and quality of NGS-based tools, diagnostics, and therapeutics among different social classes and countries.
Q: What do you see as the next horizon with NGS and oncology?
SHK: Acceptance of NGS technology in clinical practice will be unavoidable in the future. An excellent example is the acceptance of PCR. Twenty years ago, I didn’t believe that PCR would ever become an essential technology in clinical practices. Yet, it has. The same thing will happen to NGS technology. We are already experiencing a rapid increase in the number of requests we receive to perform NGS analysis of samples for clinical research studies at our hospital.
Q: What types of NGS cancer panels are you looking forward to using in the future?
KN: We are enthusiastic about the new TruSight Oncology 500 panel, which is more comprehensive and enables various types of biomarkers to be analyzed simultaneously. It will be ideal as the basis for developing companion diagnostics for new therapeutics. We’re looking forward to the opportunity to test and validate this panel in Korea soon.
We’d also like to see new NGS panels created with the necessary genes to categorize solid tumors into a few classes, such as solid tumor class I or II panels. New panels with clinically significant target genes for brain cancers would also be helpful for our clinical studies.
Learn more about the products and systems mentioned in this article:
Infinium Methylation Assay Overview
References
- Goodenberger ML and Jenkins RB. Genetics of adult glioma. Cancer Genet. 2012; 205: 613–621.
- Cohen A, Holmen S, and Colman H. IDH1 and IDH2 Mutations in Gliomas. Curr Neurol Neurosci Rep. 2013; 13:345.
- Garrett M, Sperry J, Braas D, et al. Metabolic characterization of isocitrate dehydrogenase (IDH) mutant and IDH wildtype gliomaspheres uncovers cell type-specific vulnerabilities. Cancer Metab. 2018. 6:4 doi: 10.1186/s40170-018-0177-4.
- Buchhalter I, Rempel E, Endris V, et al. Size Matters: Dissecting Key Parameters for Panel-Based Tumor Mutational Burden (TMB) Analysis. Int J Cancer. 2018. doi: 10.1002/ijc.31878.
- Hench J, Bihl M, Bratic Hench I, et al. Satisfying your neuro-oncologist: a fast approach to routine molecular glioma diagnositcs. Neuro Oncol. 2018. 12: 1682–1683.